Stent
A stent is a tubular mesh-like support structure for vessels, made from either metal or synthetic fibers. Stents are placed in blood vessels or hollow organs in order to help keep them patent (open). Stents are commonly placed, among other reasons, in the setting of coronary circulation disturbances due to coronary artery disease or after an acute heart attack. The severity of disease determines if a stent needs to be placed or not. The blood vessel is dilated before a stent is placed. Once inside, the stent presses against the wall of the vessel, helping to smooth its surface. Following stent implantation, a healthy lifestyle is imperative in order to prevention restenosis; this includes changes such as quitting smoking, weight control, eating a balanced diet and exercising often. It is also necessary to take long-term medications. An alternative to stent implantation is a bypass operation.
What are the different types of stents?
What are the different types of stents?
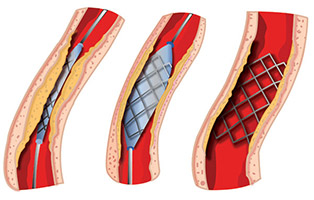
300,000 coronary stents have been placed in Germany alone, making this procedure the most common form of interventional treatment for coronary artery disease. To allow it to fit inside of a vessel, the stent is compressed so that it becomes very small. It can then be placed at the narrowest part of the blood vessel by means of a thin catheter. There are various types of stents including self-expanding or balloon-expanding, as well as medication-coated or absorbable.
Self-expanding Stents are made of metal netting surrounded by a plastic shell. They are collapsed so that they can be inserted into the vessel. Once the stent is properly placed, the shell is removed and the stent expands in order to keep the vessel open.
Balloon-expanding Stents are placed in a vessel by collapsing the stent around a balloon catheter. Once at the proper location, the balloon blows up, causing the stent to expand against the walls of the blood vessel. The vessel therefore remains open with the help of the stent.
Drug-eluting stents are stents that are coated with medications (Drug-eluting Stent, DES). These medications prevent cell regeneration, therefore preventing scar formation and restenosis (closure) of the vessel. However, not every patient requires, or is appropriate for, a drug-eluting stent. For patients with a very small occlusion (up to 10mm), the danger of restenosis is very low and a drug-eluting stent can be avoided.
An additional option is absorbable stents (Bioabsorbable Vascular Scaffold, BVS), which break down after 12 to 18 months.
When is a stent implantation performed?
A stent is placed when a vessel is unable to be kept open via simple expansion of the vessel (Percutaneous Transluminal Angioplasty). These situations may include the following:
- Circulation problems of the arteries of the extremities (Peripheral artery disease, PAD)
- Expansion of the Aorta (Aortic aneurysm)
- Stroke due to narrowing of the carotid arteries (Carotid stenosis)
- Narrowing of the arteries of the kidneys (Renal artery stenosis)
- Narrowing of ducts (i.e. Biliary tract stenosis)
- Narrowing of coronary arteries (Coronary artery disease, CAD)
Blood vessels may become closed off due to calcification of the arteries (atherosclerosis). For more information about atherosclerosis and how it occurs, read our specialty article entitled Heart Attack.
How is a stent placed?
A general examination of the patient is first carried out, in which an ECG and blood tests are performed. Additional tests such as a stress ECG, cardiac ultrasound and x-ray of the lungs and heart may be performed to obtain additional information regarding the patients overall state of health.
If a coronary artery occlusion is suspected, a cardiac (heart) catheterization is performed. In this procedure, a catheter enters the arterial circulation via an access point in the groin or occasionally in the wrist. The catheter (also known as the “guide catheter”) follows the path of the arteries until reaching the desired coronary artery. This entire process occurs under x-ray guidance. Via injection of a contrast substance, the narrowed portion of the artery can be visualized. The severity of the occlusion can then be assessed and it can be determined if a stent should be placed.
A thin wire is first inserted, making it possible for a collapsed stent to be placed via a balloon catheter directly into the narrowed area. Once in the desired location, the balloon is filled with a saline solution to create pressure, causing the stent to dilate. The balloon presses against the depositions and calcifications of the vessel wall, restoring it to its normal diameter. The balloon is emptied after approximately 30 seconds, leaving the expanded stent behind. The stent grows with the vessel wall over time and works against the formation of a new occlusion. The diameter of an expanded stent is between 2.5 and 4.0 mm.
Following stent placement, the access point is typically closed immediately following the procedure (but sometimes on the day after).
What happens following stent placement?
After the procedure, monitoring in the form of an ECG and blood tests are performed. When no complications are present the patient can be released on the next day. As a stent is a foreign body, medications must be taken to prevent blood clot formation on the surface of the stent. Stents that are covered with a synthetic membrane heal very slowly and require medications (blood thinners) to be taken for up to 12 months. Medications include those such as Plavix, Iscover or Tiklyd. Patients with drug-eluting stents must take medications for six months; those with uncoated stents should take a blood thinner for four weeks. If the medications are suddenly discontinued, an abrupt occlusion of the vessel can occur, a so-called stent thrombosis.
Monitoring is typically recommended six months after the procedure in the form of a cardiac catheterization, as narrowing can reoccur via scarring inside of the stent. If this is the case, a balloon-dilation is performed. If pain occurs within the first six months after the intervention, a catheterization may need to be performed at an earlier time.
Following all types of stent implantation, certain medications (such as Aspirin) must always be taken and regular routine check-ups must be performed. During the check-up, a stress ECG and cardiac ultrasound are performed. This helps to assess if a new vessel occlusion is present and how the heart is functioning.