Diabetes Mellitus
Diabetes mellitus – what you need to know
What types of Diabetes are there?
What are the potential consequences of Diabetes?
Diabetes mellitus – What you need to know
Diabetes mellitus is a chronic metabolic disorder, characterized by an elevated blood sugar level (hyperglycemia). The risk for severe comorbidities and potential consequences is high.
For the body to have energy it requires glucose. A certain amount of glucose is always present in the blood, which can be made available at any time (for example, in situations of sudden stress). The so-called blood sugar level (blood glucose level) of a healthy individual is normally between 80 and 120 milligrams per deciliter (mg/dl).
After eating, the Pancreas releases the hormone Insulin so that glucose can be absorbed. Insulin is produced by the Beta cells in the islets of Langerhans, which are located throughout the Pancreas. Insulin aids in the removal of glucose from the bloodstream by binding to the surface of cells, allowing them to absorb glucose. When a deficit of Insulin is present, sugar remains in the bloodstream, the blood glucose level rises and the body resorts to its fat stores as a source of energy, which can lead to further problems.
What types of Diabetes are there?
Along with rare forms of Diabetes, i.e. Gestational (pregnancy-associated) Diabetes, there are two main forms: Type 1 and Type 2. Type 1 is much less common than Type 2, with approximately 95% of cases being classified as The latter. Diabetes Mellitus is often colloquially called a „sugar disease.“ This term stems from the fact that Diabetics excrete sugar in their urine.
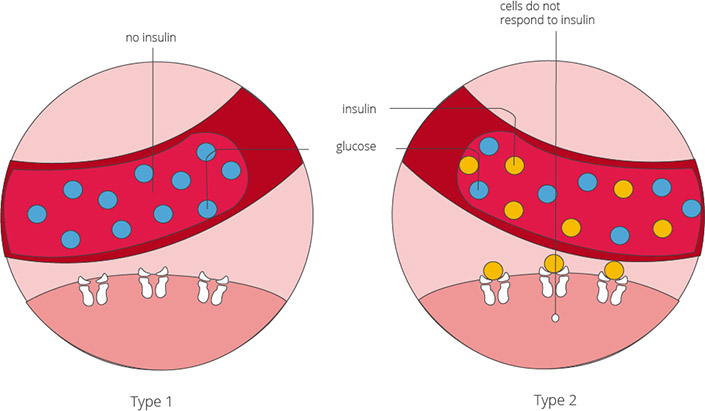
Type 1 Diabetes
This form of Diabetes often starts in childhood or as a young adult, typically between the ages of 11 and 13, and is due to a deficiency of the hormone Insulin. While the exact cause is unknown, the body’s own immune system often destroys the insulin-producing Beta cells in the, causing not enough glucose can be taken up by the cells. This process may be the result of a hereditary predisposition and certain environmental factors (i.e. viral infections such as measles or mumps).
Symptoms of Type 1:
The symptoms of Type 1 Diabetes first arise when 80% of the insulin-producing cells are destroyed. Symptoms include:
- Strong thirst
- Increased urination
- Ravenous hunger
- Itching
- Fatigue
- Susceptibility to infections
The time between the onset of disease and the presentation of symptoms can be weeks, months, or also years.
Those affected by Type 1 Diabetes must regularly inject themselves with Insulin in order to compensate for their deficiency of this hormone. The disease progresses until all of the insulin-producing cells are affected, and the body no longer produces any of its own insulin.
Type 2 Diabetes
Type 2 Diabetes affects mostly older individuals and is therefore often known as „Adult-onset Diabetes.“ The age of onset of Diabetes has, in more recent years, decreased, with more young people (including children) being diagnosed with Type 2 Diabetes. In Type 2 Diabetes, the body’s cells are less susceptible to insulin secreted by the Pancreas; this causes the blood glucose level to rise. In order to compensate and maintain a blood sugar level within a normal range, the pancreas produces more insulin. After many years, and a heavy burden on the insulin-producing cells, the production of insulin also decreases. Factors that cause insulin resistance include a high-fat diet, obesity (especially in the abdominal area), high blood pressure and lack of exercise. Those with a genetic predisposition must be particularly cautious to lead a healthy lifestyle.
Symptoms of Type 2:For a long time this disease often goes unnoticed, with symptoms arising typically only once complications arise.
What are the potential complications of Diabetes?
If the blood glucose level remains uncontrolled, the blood vessels can become damaged and further complications may arise. These include:
- Changes of the Retina (Diabetic Retinopathy)
- Disruption of kidney function (Diabetic Nephropathy)
- Heart Attack
- Stroke
- Erectile Dysfunction
- Susceptibility to infections
- Circulation problems of the legs and feet
Once numbness or paresthesia is present, Diabetes can cause permanent nerve damage. It is therefore imperative to adopt a lifelong and cautious approach to blood sugar management.
The most common complication of Diabetes is diabetic foot. Nerve damage and circulation problems in the feet lead to open, poorly healing wounds and ulcers.
It is important to note, however, that complications from Type 2 Diabetes can be prevented if a lifestyle change is adopted early on in the disease. Frequent activity, maintaining a normal weight and healthy eating can help stabilize the blood sugar level. If the disease has already progressed, medications or insulin injections must be prescribed in order to regulate the blood sugar level.
