Heart Failure
Cardiac insufficiency, more commonly known as heart failure, is when the heart muscle’s pump function is reduced. This leads to the heart being unable to produce the power to pump the required amount of blood throughout the body. In Germany alone, approximately 2 million people suffer from heart failure. In people over 70 years old, every eighth person is affected, with men typically being affected at a significantly younger age than women. The risk for men is approximately one and a half times higher than that for women. In Germany heart failure is the fourth most common cause of death among men, and the second most common cause of death among women.
What are the different types of heart failure and what are their symptoms?
Into which classes is heart failure divided?
How is heart failure diagnosed?
What are the chances of recovery from heart failure?
What is heart failure?
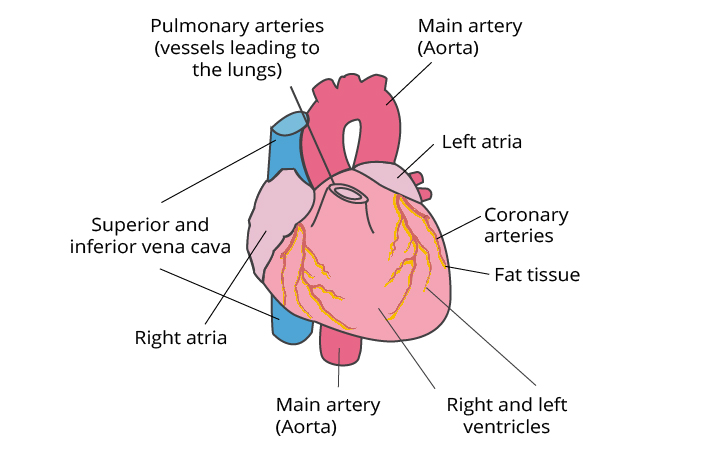
With a healthy heart, oxygen-rich blood from the left ventricle is pumped through the body to the organs to provide them with oxygen and nutrients. After supplying the organs, the oxygen-poor blood flows back from the body to the right side of the heart, from where it is transported to the lungs. In the lungs, the blood is enriched with oxygen so that it can once again be pumped throughout the body via the left ventricle.
Heart failure is a weakening of the heart’s pumping function. It typically affects either the right side of the heart (right-sided heart failure) or the left side of the heart (left-sided heart failure). In advanced heart failure, both sides of the heart can be affected (global heart failure). Heart failure can also be either chronic or acute in nature. Chronic heart failure is an advance disease that has been present for weeks, months or years and is more common than acute heart failure, which occurs suddenly and unexpectedly. Acute heart failure can suddenly stem from chronic heart failure.
What causes heart failure?
Heart failure is caused by diseases that affect or damage the heart muscle. The most common cause of chronic heart failure is coronary artery disease, particularly after a heart attack.
Coronary artery disease (CAD) is triggered by the narrowing of the coronary blood vessels (coronary arteries), most commonly due to atherosclerosis. The coronary arteries are the vessels that provide the heart with oxygen and other important nutrients. Progressive narrowing (also called stenosis) of the arteries leads to circulation disturbances of the heart muscle. CAD is often first recognized when angina pectoris (chest pain and tightness) is present, but otherwise it remains unnoticed.
A heart attack is due to a decrease in circulation of oxygen-rich blood to the heart muscle, causing the tissue to irreversibly die. This damage affects the pump function of the heart, leading to heart failure. A large portion of those affected also suffer from high blood pressure, which additionally intensifies the situation.
High blood pressure (hypertension) is the sole reason for heart failure in up to 20% of individuals, making it the second most common cause of this disease. High blood pressure causes an increased resistance, thereby making the heart continuously pump harder. The heart is unable to perform under this additional stress over a long period of time, and therefore loses some of its capacity.
A similar effect can be caused by a heart valve problem. Through narrowed or leaky aortic valves, the heart must pump stronger or beat more frequently, which also leads to a chronic increased burden.
Heart rhythm disorders such as a heart rate that is too low (bradycardia), can also be the trigger of heart failure, as too little blood is circulated. A heart rate that is too rapid (tachycardia) is associated with decreased stroke volume and can therefore also lead to heart failure.
Hereditary diseases of the heart that lead to an increase in muscle mass, can be the cause of heart failure. Pregnancy, autoimmune disorders, alcohol, drugs, or misuse of medications, heart rhythm disorders and an overactive thyroid, as well as metabolic disorders (diabetes mellitus) can all be causes of heart failure.
What are the types of heart failure and what are their symptoms?
- Left-sided heart failure
- Right-sided heart failure
- Global heart failure
- Systolic heart failure
- Diastolic heart failure
- Chronic heart failure
- Acute heart failure
Each type of heart failure has different symptoms, and the symptoms can vary in intensity. However, the main symptom of heart failure is difficulty breathing with physical activity. Warning signs may include sweating with mild physical activity, the inability to lie flat, chest tightness or presence of leg swelling.
Left-sided heart failure
The left side of the heart is responsible for pumping oxygen-rich blood throughout the body to the organs. In left-sided heart failure, the pump function of the left ventricle is restricted, causing not enough oxygen-rich blood to be pumped throughout the body. The blood instead backs up just beyond the right ventricle in the pulmonary circulation which can lead to fluid in the lungs (pulmonary edema), difficulty breathing, throat irritation, a “rattling” sound when breathing, weakness, or dizziness
It is most often caused by coronary artery disease (CAD), high blood pressure, or heart attack, and less frequently by a disorder of the heart muscle or heart valves.
Left-sided heart failure can present acutely or may develop over time. When developing over time, it is usually first noticed when physical activity causes shortness of breath. When severe, it may even lead to shortness of breath and hypotension (low blood pressure) when at rest.
Right-sided heart failure
The right side of the heart is responsible for returning oxygen-poor blood back to the lungs so that gas exchange can occur. In right-sided heart failure, the right ventricle does not work properly, causing blood that is flowing back to the heart from the body to back up in front of the heart. This causes an increased pressure in the veins, forcing fluid into the surrounding tissue. This leads to water retention, or so-called edema, particularly in the feet, toes, ankles and shins. People often notice edema when taking off tight socks and seeing the imprint still visible on their skin. It can also lead to a severe need to urinate at night when fluids return to normal circulation and the kidneys receive better circulation.
The cause is most often an acute or chronic increase in resistance of the pulmonary circulation. This resistance stems from pulmonary diseases such as pulmonary emboli, asthma, pronounced emphysema, chronic obstructive pulmonary disorder (COPD, most often due to tobacco use) or from left-sided heart failure. Rare causes include heart valve problems or heart muscle diseases.
Global heart failure
When both the left and right sides of the heart are affected, this is known as global heart failure. Symptoms of both left- and right-sided heart failure are present.
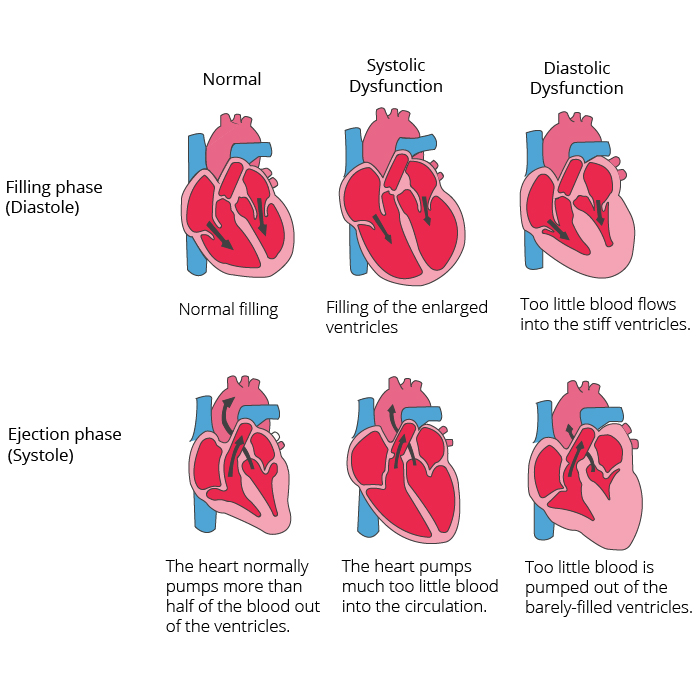
Systolic and diastolic heart failure
Systolic heart failure deals with an impaired pump or ejection performance (ejection fraction) of one or both ventricles. This occurs due to the loss of normal functioning heart muscle cells or external disturbances of the pump function. Blood backs up in the lungs and the organs do not receive an adequate amount of oxygen.
In diastolic heart failure, the heart’s ability to pump is not impacted, but the elasticity of the ventricle is impaired, causing it to not relax and refill appropriately. One of the most common causes of diastolic dysfunction is high blood pressure. Through the increased resistance in the arteries, the heart must pump harder, thereby making the heart muscle thicker and harder. The elasticity of the heart muscle is reduced, and less blood can be pumped between contractions from the ventricles into the body. This causes the body to not receive enough blood and nutrients. A heart valve disease can also lead to thickening of the heart muscle. The heart musculature becomes stiffer and less elastic due to storage of proteins. The symptoms of diastolic heart failure may be as simple as coughing, and as severe as difficulty breathing (dyspnea).
Chronic and acute heart failure
Chronic heart failure is a progressive disease that has been present for weeks, months or years, and occurs more often than acute heart failure. In chronic heart failure, the symptoms are often not taken seriously, as the body has been able to compensate over a long period of time, or the symptoms are attributed to increasing age. The symptoms reflect either left or right-sided heart failure.
Acute heart failure occurs suddenly, within minutes or hours, after a heart attack or a chronic period of heart failure, when the body can no longer compensate. Some symptoms include:
- Strong difficulty breathing and/or coughing
- Bubbling sound when breathing
- Rapid heart rate
- Pallor
- Breaking out in cold sweats
Into which classes is heart failure divided?
According to the New York Heart Association (NYHA) Functional Classification, heart failure is divided into classes I-IV dependent upon the severity of symptoms and limitation on physical activity.
Heart failure is divided into four classes dependent upon the severity of symptoms:
- NYHA I: Heart disease without any limitation of physical activity. Normal activity does not cause increased exhaustion, palpitations or difficulty breathing.
- NYHA II: Heart disease causing a mild limitation in daily activities with physical activity. No symptoms when at rest.
- NYHA III: Heart disease causing a marked limitation in daily activities. Simple activities such as brushing teeth, eating or talking cause exhaustion, palpitations or difficulty breathing. No symptoms at rest.
- NYHA IV: Heart disease causing symptoms at rest (and with any amount of mild physical activity).
How is heart failure diagnosed?
Diagnosis begins with a comprehensive evaluation of the individual’s medical history paying particular attention to symptoms (beginning, duration, manifestation). This helps to classify the symptom’s severity using the New York Heart Association (NYHA) Classification. The heart and lungs are examined. If there is suspicion of a heart attack (acute or old) or rhythm disorder, a 12-lead resting ECG is performed. Furthermore, an echocardiograph and general blood tests are performed. The necessity for catheterization is decided on an individual basis.
How is heart failure treated?
With chronic heart failure, medications (such as ACE Inhibitors, Beta Blockers and Diuretics) are implemented. Medications are used to prevent complications and improve quality of life. ACE Inhibitors and Beta Blockers can be life prolonging, but must be taken regularly and chronically to have this effect.
Additionally, rhythm therapies (for treatment of heart rhythm disorders) or three-chamber pacemakers are also used. The latter provides for timely activation of the atria and both ventricles. A defibrillator is also often implanted as part of the pacemaker to counteract dangerous heart rhythm disorders in the setting of severe heart failure. This treatment is also known as resynchronization therapy. Physical therapy is also an important part of successful treatment.
What are the chances of recovery from heart failure?
Heart failure is unable to be “cured.” However, the life expectancy of those affected can be significantly improved. This is dependent upon the type of heart failure, as well as the age, comorbid illnesses and lifestyle of the individual. If comorbid conditions (such as high blood pressure) are treated, a healthy lifestyle is followed and doctor’s recommendations are adhered to, a good long-term prognosis is possible.