Heart Attack (Myocardial Infarction)
Heart attack (myocardial infarction) is one of the most common forms of cardiovascular disease. 400,000 people in Germany alone suffer from a heart attack each year, affecting individuals of all ages. The amount of time that elapses between when a heart attack occurs and when treatment is received is critical in determining the individual’s outcome. According to the American Heart Association, every 30 minute delay in treatment increases mortality by 7,5%. It is therefore important to seek medical attention upon the first suspicion of a heart attack.
What are some symptoms of a heart attack?
How is a heart attack diagnosed?
What are some risk factors for atherosclerosis and heart attack?
You know how old you are, but do you know how old your heart is?
What is a heart attack ?
The heart is supplied with oxygen by blood vessels (coronary arteries) that cover the heart. A heart attack is present when a blood vessel is blocked, which typically occurs due to a blood clot in an already narrowed portion of the artery. The heart uses 5-20% of the body’s oxygen supply (dependent upon physical performance) to pump blood throughout the body. If the heart does not receive enough oxygen, a part of the heart muscle dies. This can occur as early as within twenty minutes. In severe cases the heart is damaged to such an extent that the person dies.
In cardiology, the “golden hour” is frequently referenced when talking about heart attacks—this term emphasizes the importance of receiving treatment within one hour to limit damage to the heart. When treatment is received too late heart muscle dies irrecoverably, scar tissue is formed, also increasing the risk for other heart disorders such as arrhythmias. Arrhythmias can impact the ability of the heart to effectively pump blood throughout the body; in severe situations, they can even lead to cardiac arrest.
What causes a heart attack?
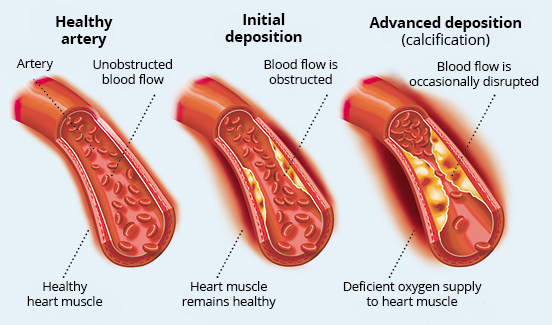
Atherosclerosis is a chronic disease causing calcification of the arteries and is the usual cause of a heart attack.
Arteries are blood vessels that carry oxygen-rich blood from the heart to the organs, muscles and tissues. When the inner layer of the arteries is damaged (from high blood pressure, smoking or high cholesterol), excess “bad fat,” or LDL cholesterol, circulating in the blood stream attaches to this area. This then attracts white blood cells (macrophages); the white blood cells and LDL cholesterol form a plaque within the vessel wall, causing the artery to lose its normal elasticity. The arteries become narrower and more rigid over time, causing a disturbance in circulation and may even become completely blocked.
If the surface of a plaque ruptures, platelets (thrombocytes) that are flowing by in the bloodstream attach themselves to this area and form a clot (thrombus). This blocks the blood vessel causing an occlusion. When the vessel is blocked, the circulation is affected, causing an inadequate amount of oxygen to be delivered to the heart muscle. If the blocked vessel is not quickly reopened, the muscle receiving its blood supply from this artery dies and forms scar tissue.
Atherosclerosis can affect blood vessels of the heart, brain, neck and extremities. When a vessel in the legs is affected, this causes peripheral artery disease; when an artery in the brain is occluded, this leads to a stroke. The blood vessels surrounding the heart are called the coronary arteries- when these are affected by atherosclerosis, it is known as coronary artery disease (CAD). When a coronary artery is blocked, this causes a heart attack.
In addition to blood clots, blood vessel spasms (coronary artery spasms), coronary artery emboli, or restenosis of a stent or coronary bypass graft can lead to a heart attack. Stents are wire nettings that are placed in the coronary blood vessels to keep a narrow portion of the vessel patent.
What are some symptoms of a heart attack?
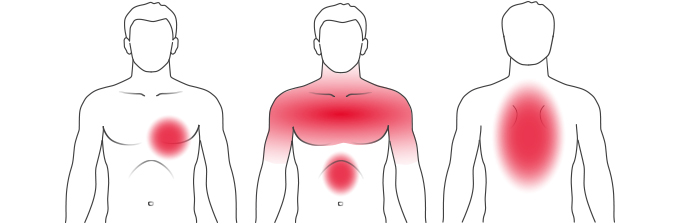
A heart attack often occurs in situations with a high level of stress or physical exertion, as these lead to an increase in blood pressure and heart rate, as the blood vessels are narrower. However, many infarcts also occur in the early hours of the morning when the body is at rest. Most patients who have a heart attack already suffer from coronary artery disease. When the heart muscle is not receiving enough oxygen, strong chest pain or a sensation of pressure behind the sternum may occur. A physician should be seen immediately for evaluation.
Often, however, symptoms are indistinct which causes those suffering to not link their symptoms to a heart problem. The confusion associated with how to manage symptoms causes a delay in seeking treatment that can lead to valuable heart muscle dying irreversibly. The earlier that you seek treatment, the higher the chances of a good recovery.
Possible symptoms of a heart attack may also include:
- Sudden occurrence of pain
- Presence of pain lasting longer than five minutes
- Pain radiation to either arm, the upper stomach, the jaw and/or the back (between the shoulder blades to the neck)
- Anxiety
- Difficulty breathing
- Pallor
- Chest tightness
- Fainting or shock
- Racing heart
- Cold sweats
- Feeling of uneasiness
- Nausea or vomiting
- Dizziness
What is important to know?
It is important to note that symptoms of a heart attack are not always obvious and their intensity may vary from person to person. In addition to typical pain in the chest, sudden neck, jaw, back or upper abdominal pain may also be symptoms of an infarct. There are also heart attacks that present without any symptoms at all, so-called “silent heart attacks.” These are typically only discovered during a later examination with an ECG or when side effects are present.
Women tend to experience classic symptoms less often than men, but more often perceive a strong pressure or tightness in the chest, as well as nausea, vomiting, difficulty breathing and pain in the upper stomach. Some precursors, which may present weeks in advance include severe fatigue, sleep disturbances or difficulty breathing. Read more about heart attacks among women in our specialty article.
If you suspect someone is having a heart attack, the following should be done:- Do not waste any time— call your physician or your respective emergency medical phone number immediately
- Have the patient sit or lie down, with the upper body slightly elevated to relieve the burden on the heart
- Keep the patient calm and loosen any tight clothing
- Observe the breathing and circulation (pulse)
- If the patient stops breathing or his/her pulse becomes absent, begin CPR immediately
Emergency medical personnel will administer medications to help relieve the burden on the heart. These may include medications for pain (to treat the patient’s symptoms), to dilate the blood vessels (to improve circulation) and or to thin the blood. Various tests and procedures are performed in the clinic or hospital for diagnosis and treatment.
How is a heart attack diagnosed?
If a heart attack is suspected, the patient’s medical history will be taken and a physical examination is performed. The quickest way of assessment is by means of an ECG (electrocardiogram), which allows for a full diagnosis, and in many cases can tell which part of the heart is affected. An ECG can be performed, as commonly known, at the doctor’s office or hospital. However, it is also now possible to perform profound ECGs at home using mobile devices that provide information on the status of the heart’s health. In addition, blood tests are performed which can provide information such as if heart tissue has been damaged, thereby confirming the ECG assessment, and the approximate time when the heart attack started. These blood tests include cardiac Troponin-T and Troponin-I. The levels of these markers in the blood rise within a few hours after a heart attack; when elevated they indicate damage to the heart muscle. An Echocardiograph (cardiac ultrasound) is also performed, which can paint a general picture of how the heart is functioning and give an idea how large the infarct is. A cardiac catheterization assesses the severity of the coronary vessel occlusion. When it is determined during the examination that intervention is needed, a stent can be immediately placed. Magnetic Resonance Imaging (MRI) can also provide additional information regarding the extent of the damage and the effect on the heart’s circulation.
What are some risk factors for atherosclerosis and heart attack?
Risk factors for atherosclerosis (blood vessel calcification) are divided into factors that can be influenced, and those that cannot be. Risk factors that we can help control include high blood pressure, diabetes mellitus, obesity, sleep apnea and lipid disorders (such as elevated LDL cholesterol). You can read more about these risk factors in our Specialty Articles. Unhealthy nutrition, being overweight, lack of exercise and stress all have a negative influence on our bodies. A healthy lifestyle can help to reverse the impact of these risk factors and prevent negative side effects.
A factor that we cannot influence is genetics. If a first degree relative (sibling or parent) experienced a heart attack or underwent a cardiac bypass operation before turning 60, an elevated risk is present.
Circulation problems can be the result of high blood pressure. How this happens and its effects can be read about in our specialty article High Blood Pressure.
You know how old you are, but do you know how old your heart is?
The heart is one of our most important organs and is greatly influenced by our lifestyle. Our eating habits, weight, age, physical fitness level and prior medical history have a strong impact on our hearts and may cause premature aging. Find out how old your heart actually is with our Heart-Age Calculator.


